
Журнал "Медицинский совет" №16 2018
Ю.А. Карпов, ФГБУ «Национальный медицинский исследовательский центр кардиологии» Минздрава России, г. Москва
Рациональное сочетание медикаментозного и инвазивного ведения больного стабильной ИБС позволяет значительно снизить риск сердечно-сосудистых осложнений и улучшить качество жизни. Новые технологии могут значительно улучшить результаты лечения этих пациентов только при условии соблюдения предписанных врачом схем. Между тем приверженность сердечно-сосудистой терапии низкая, а задача ее повышения, в частности регулярное применение антиагрегантных препаратов и статинов, весьма актуальна. Одним из эффективных методов улучшения приверженности является назначение фиксированных комбинаций лекарственных препаратов.
Coronary heart disease: how to improve the effectiveness of treatment?
Karpov Yu.A., National medical research center of cardiology, Ministry of health of Russia
A rational combination of drug and invasive management of a patient with stable coronary artery disease can significantly reduce the risk of cardiovascular complications and improve the quality of life. New technologies can significantly improve the results of treatment of these patients only if the prescribed regimens are followed. Meanwhile, adherence to cardiovascular therapy is low, and the task of its increase, in particular the regular use of antiplatelet drugs and statins, is very relevant. One of the effective methods of improving adherence is the appointment of fixed combinations of drugs.
Загрузить
Список литературы
1. Клинические рекомендации. Стабильная ишемическая болезнь сердца. 2016. http://www.cr.rosminzdrav.ru/clin_recomend.
2. 2013 ESC Guidelines on the management of stable coronary artery disease. The Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J, 2013, 34: 2949-3003.
3. 2016 ESC/EAS Guidelines for the мanagement of dyslipidaemias. Eur Heart J, 2016, 37: 2999-3058.
4. Диагностика и коррекция нарушений липидного обмена с целью профилактики и лечения атеросклероза. Российские рекомендации (VI пересмотр). М., 2017
5. Cannon CP, Blazing MA, Giugliano RP et al, IMPROVE-IT Investigators. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med, 2015, 372: 2387-2397.
6. Mombelli G, Castelnuovo S, Pavanello C. Potential of PCSK9 as a new target for the management of LDL cholesterol Research Reports in Clinical Cardiology 2015, 6: 73-86.
7. Sabatine MS, Giugliano RP, Pedersen TR. Evolocumab in patients with cardiovascular disease. N Engl J Med, 2017, 377: 787-788.
8. Steg PG, et al. Odyssey outcomes study: main results. ACC, 67th annual scientific session. Orlando, March 10, 2018.
9. Томилова Д.И., Карпов Ю.А., Лопухова В.В. Долгосрочная приверженность терапии статинами после планового коронарного стентирования при стабильной стенокардии. Кардиология, 2018, 5: 5-10.
10. Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med, 2012, 125: 882-887.
11. Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst Rev, 2010, 3: CD004371.
12. Antithrombotic Trialists (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative metaanalysis of individual participant data from randomised trials. Lancet, 2009, 373: 1849-60.
13. Sundström J, Hedberg J, Thuresson M, Aarskog P, Johannesen KM, Oldgren J. Low-Dose Aspirin Discontinuation and Risk of Cardiovascular Events. A Swedish Nationwide, PopulationBased Cohort Study. Circulation, 2017, 136: 1183-1192.
14. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J, 2018, 39: 119- 77. https://doi.org/10.1093/eurheartj/ehx393V.
15. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J, 2018, 39: 763-821.
16. Luvai A, Mbagaya W, Hall AS, Barth JH. Rosuvastatin: a review of the pharmacology and clinical effectiveness in cardiovascular disease. Clin Med Insights Cardiol, 2012, 6: 17-33.
17. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTSThe Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J, 2017 https://doi.org/10.1093/eurheartj/ehx419.
18. Bonaca MP, Bhatt DL, Cohen M, Steg PG, Storey RF, Jensen EC, Magnani G, Bansilal S, Fish MP, Im K, Bengtsson O, Oude Ophuis T, Budaj A, Theroux P, Ruda M, Hamm C, Goto S, Spinar J, Nicolau JC, Kiss RG, Murphy SA, Wiviott SD, Held P, Braunwald E, Sabatine MS, PEGASUSTIMI 54 Steering Committee and Investigators. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med, 2015, 372: 1791-1800.
19. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease. Circulation, 2012, 126: e354-e471.
20. Udell JA, Bonaca MP, Collet JP, Lincoff AM, Kereiakes DJ, Costa F, Lee CW, Mauri L, Valgimigli M, Park SJ, Montalescot G, Sabatine MS, Braunwald E, Bhatt DL. Long-term dual antiplatelet therapy for secondary prevention of cardiovascular events in the subgroup of patients with previous myocardial infarction: a collaborative meta-analysis of randomized trials. Eur Heart J, 2016, 37: 390-399.
21. Eikelboom JW, Connolly SJ, Bosch J et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med, 2017, 377: 1319-1330.
22. Boden WE, O’Rourke RA, Teo KK, et al. Group CTR. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med, 2007, 356(15): 1503-16.
23. Sedlis SP, M.D., Hartigan PM, Teo KK, et al for the COURAGE Trial Investigators. Original effect of PCI on long-term survival in patients with stable ischemic heart disease. N Engl J Med, 2015, 373: 1937-1946.
24. Gada H, Kirtane AJ, Kereiakes DJ, et al. Metaanalysis of trials on mortality after percutaneous coronary intervention compared with medical therapy in patients with stable coronary heart disease and objective evidence of myocardial ischemia. Am J Cardiol, 2015, 115: 1194-1199.
25. Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet, 2017 Nov 1. pii: S0140-6736(17)32714-9. https://doi.org/10.1016/S0140-6736(17)32714-9.
26. Карпов Ю.А., Козловская И.Л., Булкина О.С., Лопухова В.В. Чрескожное коронарное вмешательство: какие вопросы решаем? Российский кардиологический журнал, 2018, 3(155): 7-10.

 1
1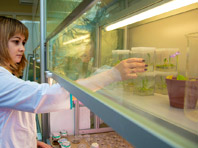 2
2 3
3 4
4
Комментарии (0)